When APD’s pain clinic began seeing patients for pain procedures in the post anesthesia care unit (PACU) procedure room during the summer of 2023, it wasn’t long before Laura Hamilton, RN, Director of Perioperative Services, began to see ways to offer more benefits to patients.
Initially, pain clinic nurse Tiffany Munn, RN, performed every role, such as showing patients to their rooms, helping them get ready for their procedures, and documenting readiness for surgery, events of the procedure, and how the patient is recovering. “I felt we could operationalize tasks by bringing patients into the perioperative arena,” Laura said.
Following a successful launch, the perioperative team, together with the pain clinic, set another goal: to perform pain procedures such as cervical or C-spine injections or radio-frequency ablations (RFAs) in the Procedure Room.
But patients who are frightened about having injections require sedation during procedures and recovery space when complete. These patients would also require a different workflow, including a robust nursing assessment. PACU nurse Elizabeth Bergeron, BSN, RN, was ready for the challenge.
“When asked if we would help create this type of experience for pain injection patients, we jumped at the chance,” Elizabeth said. “Not only are we creating a comfortable experience for our patients, but these procedures allow APD’s perioperative nurses to practice at the top of our abilities.”
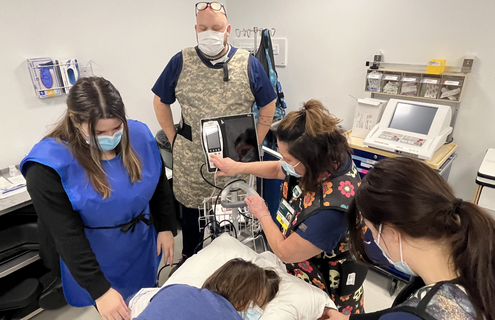
Pain clinic patients are now seen in the Procedure Room once a month. Tiffany supports with patient positioning, medication prep, cleaning the injection site, managing supplies, and running the RFA machine. A perioperative nurse preps the patient. Tiffany remains with the rest of the team in the procedure room for support during the case, while Elizabeth or Crissie Bean, RN, administers IV medication during the procedure. Finally, the patient goes to the recovery room with a PACU nurse.
The new procedures provide learning opportunities for the perioperative team. For example, the teams needed nurses trained to administer sedating medications, so APD’s perioperative nurses are pursuing conscious sedation certification (CSRN).
“This work encourages growth in our same day surgery nursing skillset while also using the diverse skills we already have,” Elizabeth said.
It allows more access to APD for patients who wish to receive all of their care here. Previously, RFA patients might have undergone a diagnostic procedure at APD, followed by an RFA at Dartmouth Hitchcock Medical Center.
“Now that APD has the process and skills to support this, patients receive medication so they can tolerate the procedure and be treated in a facility they know, trust, and feel comfortable in,” Laura said. “They tell us constantly, ‘I’m so glad I was able to have this done at APD.’”